This article is not yet available in the language you selected
Pathogenic viruses in our food
Article index
Viruses are outsiders in (micro)biology. Strictly, viruses aren’t living creatures, as they have no metabolism. They are somewhere between living and non-living material. They are particles having genetic material (DNA or RNA) encapsulated with a protein coat. Some viruses have a supplementary lipid coat, named envelope. Viruses are spherical, rod-shaped, isometrical or phage-type viruses existing of a head, genetic material, a tail and a base plate with spines or tail threads. Their magnitude is 20-400 nm, and they can only be observed with an electronic microscope. Viruses can’t grow in foodstuffs. They can only survive. Multiplication occurs in the somatic cells of their guest.
Virusen are observed in plants, animals and bacteria. They can be transfered to humans in some cases. Recent damage caused by pork fever, chicken fever and herpes to local economies, and the threat of human health by SARS- and chicken fever made that virology becomes an
important research field.
| Reasons why the number of food infections is increasing |
|
|
|
|
|
|
|
|
Food with the largest contamination risk
Contamination occurs via infected persons, by irrigation of plants via virus-contaminated water, by rinsing food with contaminated rinse water, by pollution of the cultivation grounds of crustaceans. Especially raw food, cold food and crustaceans are involved in viral food infections. Salads, baked goods, desserts, raw cutted vegetables and fruit, poultry, frozen raspberries and especially drinking water and crustaceans are important sources of viral food infections. As crustaceans filtrate water, virus particles are concentrated in these species. Crustaceans that contain faecal indicator organisms, are often rinsed with pure seawater to reduce that contamination. This is effective to reduce the bacterial contamination, but less succesfull to reduce viral contamination. As crustaceans are eaten raw or as they are only slightly heated, viruses can infect their guest.Noroviruses
Norovirussen, in the past named Norwalk-like viruses or Small Round Structured Viruses (SRSV), belong to the family of enteral caliciviruses. They cause epidemic gastro-enteritis in human, the whole year, with a peak during winter months. During the winther months, oysters undergo physiological changes making them more prone to take in virus particles.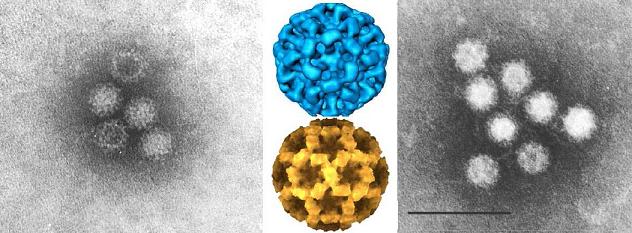
In adults, the symptoms start after 1 to 3 days: abdominal pain, projectile vomiting and diarrhoea without blood or mucus. Dehydration is the most frequent complication. When the symptoms disappear, the patient still feels weak for 2-3 weeks.
Only a small number of virusparticles (10-100) are needed to make somebody ill. Viruses multiply in the intestines to large numbers that become excreted during vomiting or via the faeces (in most cases 10 million viruses per gram vomit or faeces).
About 10-20 % of the norovirus-infectieons occur via contaminated food or water. Products like fresh fruits (blueberries and raspberries), salads, crustaceans, eggs, cooked food, drinks and covered sandwiches are risky to eat. More than other food, crustaceans are involved in the explosion of norovirus-gastro-enteritis. During extreme rainfall, feacal contamination of the oyster banks occurs as large quantities of waste water are transferred in the surface waters.
Contamination by infected employees in the food industry is another frequent cause. Man can be a vehicle of the virus without showing the symptoms. By this way, they can easily infect other people.
When taking strict hygienic measures immediately, the expansion of the norovirus can be stopped. Personel showing the signs of gastro-enteritis are advised to restart the work only 48 to 72 hours after the complaints disappear. They must wash their hands thoroughly and be very hygienic after visisting the toilet. Skirts and handshoes that are thrown away must be used.
Sapoviruses
Sapoviruses, in the past named Sapporovirussen, belong to a family of enteral calicivirussen. Especially pre-schooler and young children become ill; but adults are also easily infected.Symptoms are: abdominal pain, vomiting, diarrhoea, headache, myalgia, fever. The hygienic measures to take are the same as those applicable to noroviruses.
Enteroviruses
Enteroviruses, belonging to the family of the picornaviruses are divided in 4 categories: polioviruses, group A coxsackieviruses, group B coxsackieviruses and echo-viruses. Polioviruses cause polyomyelitis. After an incubationperiod of 5-14 days the first symptoms are seen: fever, headache, cold in the nose, sore troat, gastro-intestinal complaints (no diarrhoea, but vomiting). 11 to 17 days after infection, the first symptoms of paralysis due to damage of the nerve cells of the spinal cord are seen. Persons of all age can be infected with the poliovirus via faecal-oral way. Especially in non-vaccinated children < 3 years old can poliomyelitis can develop. Infection occurs via food (milk, etc.) and drinking water. Food can be contaminated via hands, coughing and flies. A good hand hygiene and the treatment and conservation of food in closed recipients are the most important measures to take to avoid contamination with the poliovirus. Coxsackieviruses can cause infection via faecal-oral way. Start symptoms are respiratory and gastro-intestinal complaints, myalgia, fever, headache, soar troat, chest pain. Group B coxsackieviruses can cause myalgia, temporary paralysis, meningitis, pancreatitis and myopericarditis. Group A coxsackievirruses can infect the upper respiratory tract, can cause pharingitis, meningitis, permanent paralysis and skin rash. Echoviruses are seen in all ages, but they are especially dangerous for neonates. With age, the dying rate decreases. After an incubation period of 3-10 days, the first symptoms are observed: high fever, vomiting, diarrhoe, irritation and headache. After that myositis, hepatitis, echoviral meningitis and/or encephalitis are observed. The contamination occurs via faecal-oral way: contaminated food and drinking water. A good hand hygiene is necessary.Hepatitis A virus
Viral hepatitis caused by the hepatitis A picornavirus is observed after a long incubation period of 3 to 6 weeks. During the incubation period large numbers of viruses can spread via the urine or faeces. Symptoms are lost of appetite, general malaise, fever, headache, abdominal pain, nauseaand vomiting. Then, the skin becomes yellow due to inflammation of the liver. The duration of the illness can vary from weeks to months (fatigue during months) and for adults the disease can be more severe than for children. In special cases, the illness can be fatal for elderly. Vaccination
for hepatitis A is the method of prevention.
Hepatitis A can occur after consumption of contaminated food (salads, crustaceans, sandwiches, fruit, fruit juice, milk and dairy products, vegetables, soft drinks with ice) or after drinking water that is contaminated with the hepatitis A virus. The risk for hepatitis A is large in countries with poor hygiene: the water is contaminated, vegetables are washed with contaminated water, etc. But also in our regions, food can be contaminated with the hepatitis A virus (especially raw fish and crustaceans).
Hepatitis E virus
The symptoms of hepatitis E are about the same of that of hepatitis A. With hepatitis E the inflammation of the liver is more severe than with hepatitis A. In infected pregnant woman, hepatitis E gives increased mortality. The incubation period is 2 to 7 weeks. There is no medication against hepatitis E and a vaccin for hepatitis E neither exists.Contamination with hepatitis E-virus occurs via faecal-oral way. Water polluted with human and pork faeces is an important source of contamination. Through good hygienic measures hepatitis E can be anticipated. In many countries of North-Africa and in India hepatitis E is often observed.
Drinking water and food (especially crustaceans and pork meat) must be cooked/roasted. Pure drinking water is a necessary precaution to prevent contamination. Hands must be washed thoroughly before preparing foods and after a visit to the toilet.
Rotavirus
Rotavirus is the most observed cause of acute diarrhoea. Found in 2/3rd of the positive virus cultures, it is especially observed in neonatants and pre-schoolers. Sometimes, the virus also causes diarrhoea in travellers, elderly and attendants of young children. This diarrhoea can take a long while, as the flock atrophy recovers only after 10 days. During the first 10 days of the illness (incubation time 1-3 days) vomiting, fever and abdominal pain are frequently observed symptoms. Moreover, the virus can infect the upper respiratory tract. Through the frequent vomiting and the watery diarrhoea dehydratation is an important complication. This dehydratation is especially dangerous for children under the 2 years old.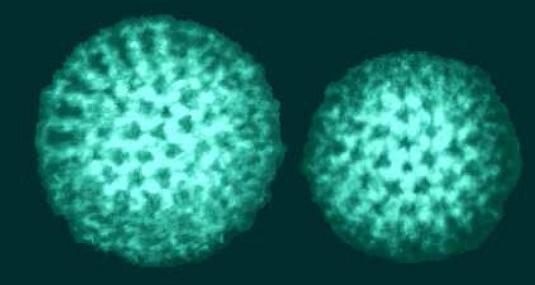
Precautions to prevent infection by the rotavirus: regular washing of hands followed by disinfection with desinfectantia, carefull cleaning and disinfection of surfaces and rooms, good hygiene with attendants of children, etc. In countries with high hygiene risk the travellers may not drink tap water or unpasteurised milk. They better consume no ice and unpasteurised dairy products, and eating in unhygienic snack bars and restaurants must be avoided. Safe for consumption are bottles carbonated soft drinks (soft drinks with a tase), beer, wine, hot coffee or tea, cooked water or water purified with jodium or chlorine.
Adenoviruses
Adenoviruses usually cause infection of the respiratory tracts. However, some types (40 and 41) cause acute gastro-enteritis with children, that in severness is comparable to a rotavirus infection. Also immunocompressed persons and adults can be infected by the adenovirus, and can suffer from gastro-enteritis. Contamination occurs along the faecal-oral route, especially after eating crustaceans. Adenoviruses are extremely resistant to physical and chemical agents, bad pHconditions, etc. By this mean, they can survive outside the body for a long time. Porks and bovines are reservoirs for adenoviruses.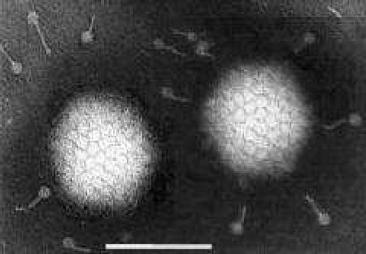
Parvovirussen
Parvovirussen cause gastroenteritis in all ages. The infection occurs especially via crustaceans contaminated with parvo-like viruses. The incubation time amounts 10 to 70 hours. The symptoms takes 3 to 9 days. They are identical to those specific for a rotavirus-infection; but they are milder.Astroviruses
After an incubation period of 3-4 days, astroviruses cause the malabsorption-syndrome, meaning incomplete absorption of food, with as consequences: abdominal pain, vomiting, diarrhoea, anemia, loss of weight, shortness in vitamins and minerals. Especially children in an age less than 4 years are victim of the virus; but also adults and elderly can be hidden.The contamination occurs via faecal-oral route. The infectuous dose is < 100 viruses Astroviruses are found in poultry, porks, sheeps, bovines and crustaceans.
Hantaviruses
Hantaviruses belong to the family of bunyaviruses. They are transferred from rodents to human. Hantaviruses are divided in two groups. The first group is found in Asia and Europe. They cause infection of the kidneys, viral hemoragic fever, bleeding and functional disorders of different organs. The viruses of the second group are only found in the United States. They are responsible for the hantavirus pulmonary syndrome. The infected victim show the following symptoms: fever, muscular pain, shiver, headache, nausea, vomiting and diarrhoea. Accumulation of moisture in the lungs cause diffulties in breathing.About 50 percent of the hantavirus infections are deadly. Therefore prevention is of utmost importance. Up to now, there is no vaccine against hantavirus infections.
Contact with rodents must be avoided. Food must be stored in closed recipients. The entrance of rodents to the factory must be avoided. All openings and cracks must be hermetically sealed. Rooms penetrated by rodents and objects they come into contact must be thoroughly cleaned and disinfected with a 10 % NaOCl-solution.
Herpes
Herpesviruses belong to the family of picornaviruses. They cause herpes with ruminates and pigs. Milk, meat and organs originating from contaminated animals can infect human beings. Although, men are infected rarely. Symptoms are: fever, vomiting, malaise, small red wounds around the mouth and vesicles on the skin. The virus survives for a long time in fresh, partially boiled, cured of smoked meat and in milk that is pasteurised unsufficiently. To avoid infection with herpes viruses, meat and milk of infected animals may not be consumed. Intense contact with sick animals must be avoided.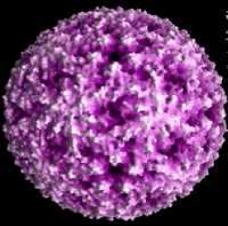
Influenza type A and rhinovirus
Influenza viruses infect the upper respiratory tracts (nose, troat and lungs), while rhinoviruses cause only a cold (sneezing and coughing). Via food, they can be transferred from one person to another. Food is contaminated via the respiration and via hands. A mask and proper hygiene are important measures. Employees must be withdrawn of their work place.SARS (Severe Acute Respiratory Syndrome) coronavirus
SARS coronavirus (SARS-CoV) irritate the respiratory tract. After an incubation period of 2 to 10 days, some influenza-like symptoms appear like fever, myalgia, gastro-intestinal problems (acute diarrhoea) and sore troat. In a second stadium, coughing and shortness in breathing are seen. Contamination occurs via faecal-oral route and via aerosols (during coughing and splashing water). The virus survives for many hours on hands and surfaces. A strict hygiene for persons involved in food production in and outside the food industry is required. During the preparation of ready meals (sandwiches, vegetable salads, etc.) and during the cutting of fruit, employees in the food industry must wear gloves that are thrown away, a hairnet, protective clothing and a mask (aerosols).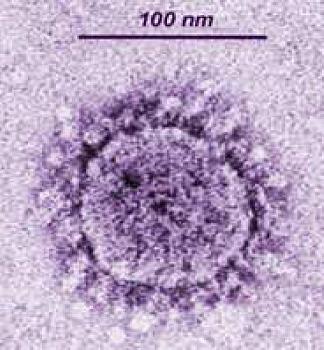
Teakningo-encefalitisvirus
Het teakmeningo-encefalitisvirus that belong to the family of flaviviruses are the only viruses that are not transferred to humans via the faecal-oral route. Teaks can be the guest of this virus type. Teaks are found in woods and long grass. To suck blood, they can attach themselves on the skin of humans and animals. After a bite of a teak, the virus can be spread in cows, goats and sheeps. Whereafter the virus is excreted in the milk of these infected animals. By this way, a consumer can be infected. Milk must be pasteurised sufficiently to avoid the outbreak of the disease. Teakmeningo-encefalitis (TBE) is a viral infection with an incubation time of 7 to 28 days. In the beginning the symptoms ressemble that of influenza: fever, headache, general malaise. This period takes about 7 days. With one third of the patients, the virus attacks the nerve system and causes inflammation of the brains (encefalitis) or inflammation of cerebral membrane (meningitis). Mortality is not excluded.Detection of virus particles in the food
Dairly research for virus infections in Belgium is not done. Only if there is any suspicion that viruses are the cause of an infection, research for the presence of viruses in the food is done.Viruses are difficult to search during routinely detection. They can not be cultivated on classic culture media of bacteria. They need a guest to multiply. The minimal detection limit is higher than 1 million virus particles per gram faeces. This means that only during the first 48 hours of a gastro-enteritis the virus particles can be demonstrated. Therefore one needs specific equipment like an electron microscope or with PCR (Polymerase Chain Reaction) and immunological tests. There is a need for fast, simple and cheap methods of detection and identification of food associated viruses.
Virus-inactivation and general prevention
In food and crustaceans, viruses are thermoresistant. A simple pasteurisation of 60°C during 30 min is not sufficient to kill the viruses. A heat treatment till an internal temperature of 85-90°C during 90 seconds is necessary, or a heat treatment of 70°C during several minutes is required. But even after heat treatment, through contamination afterwards (crosscontamination) infection can still happen. Virusen cannot be killed through cooling or freezing, neither by preservation in high sugar concentrations, alcohol or acid. Ionizing radiation and preservatives have no effect. Only disinfectants (500 ppm active chlorine) can desinactivate viruses.Food contaminated with pathogenic viruses don’t smell or taste otherwise than normal food. Regarding food safety, the consumer can’t base on sensorial characteristics. Prevention of contamination of food with pathogenic viruses is the only measure of hygiene to take.
| Prevention of food associated viral infections |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
 back to top
back to top



 companias
companias